5 min read
Friday, 3 October, 2025
Osteoarthritis is often dismissed as “just wear and tear,” but it’s much more than that. Whether you’re dealing with stiff knees or worried about your parents' joint pain, this blog walks you through everything you need to know, from osteoarthritis causes and osteoarthritis symptoms to treatments that work, to advanced therapies and the management of osteoarthritis in daily life.
No medical jargon. No sugar-coating. Just clear, science-backed, and easy-to-follow advice so you can take control of your joint health.
What Is Osteoarthritis?
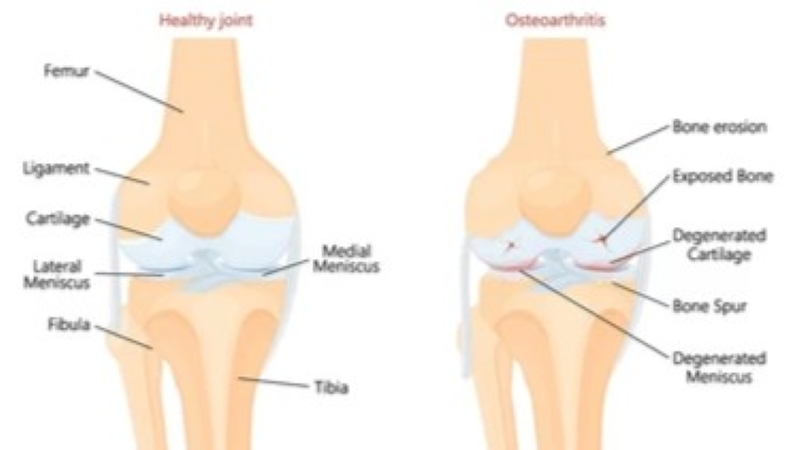
So, what’s the real osteoarthritis meaning or OA? The OA full form is osteoarthritis, which is the most common form of arthritis, affecting millions of people worldwide. Often called a “wear-and-tear” disease, it happens when the cartilage, the smooth, rubbery tissue that cushions the ends of bones, gradually breaks down.
Cartilage works like the shock absorbers in a car. When healthy, it prevents bones from grinding against each other. In osteoarthritis, this cushion wears thin, resulting in pain, stiffness, swelling, and reduced flexibility. Unlike autoimmune arthritis (such as rheumatoid arthritis), osteoarthritis is primarily a mechanical and degenerative process, although low-grade inflammation also plays a role.
Osteoarthritis vs other arthritis types
People often confuse the difference between osteoarthritis and rheumatoid arthritis or the difference between arthritis and osteoarthritis. Here’s how OA compares:
- Osteoarthritis (OA):
- Caused by cartilage wear and tear
- Usually affects older adults
- Pain worsens with activity, improves with rest
- Rheumatoid Arthritis (RA):
- Autoimmune disease where the immune system attacks joints. Treated with specialised plans like Rheumatoid arthritis exercises.
- It can affect younger adults
- Symptoms include morning stiffness lasting >1 hour, symmetrical joint pain, fatigue
- Gout:
- Caused by uric acid crystal deposits in joints
- Sudden, severe pain and swelling, often in the big toe
This comparison matters because treatment and long-term outlook differ significantly. And knowing these differences helps avoid misdiagnosis and ensures the right OA treatment.
Commonly Affected Joints in Osteoarthritis
Knee osteoarthritis
The management of osteoarthritis of the knee joint is often caused by excess weight or injury. Osteoarthritis knee symptoms include stiffness, pain, and occasional swelling. And it leads to difficulty walking, climbing stairs, and getting up from chairs.
Hip osteoarthritis
Usually results in pain in the groin, thigh, or buttocks. Daily activities like bending or putting on shoes become hard.
Osteoarthritis in hands
Causes stiffness and swelling in fingers, thumbs, and wrists. Tasks like opening jars or typing become painful.
Each area may require a slightly different osteoarthritis knee treatment or hand therapy.
Who Is at Risk?
While cartilage wear is the root cause, several factors make osteoarthritis more likely. There’s a difference between direct osteoarthritis causes and osteoarthritis risk factors:
- Age: Risk increases with age, especially after 45.
- Gender: Women, particularly after menopause, are more affected.
- Obesity: Extra body weight puts stress on the knees, hips, and spine.
- Injuries: Sports injuries or work-related joint injuries, fractures or ligament tears increase risk.
- Genetics: Some people have this query: Is osteoarthritis genetic? Family history plays a role.
- Joint overuse: Jobs or sports requiring repetitive motion strain cartilage.
It’s important to note: having risk factors doesn’t mean you’ll definitely get osteoarthritis, but it does mean you should protect your joints early. Recognising these osteoarthritis risk factors allows for early non-pharmacological management of osteoarthritis, such as exercise and diet changes.
Understanding the Stages of Osteoarthritis
Osteoarthritis doesn’t happen overnight. It progresses slowly, and doctors often use osteoarthritis classification, osteoarthritis grading, or stages of osteoarthritis to describe how advanced the disease is. To make it simpler, we have classified it into four main stages. The pathogenesis of osteoarthritis (how it develops) usually follows a stepwise pattern, which can be seen clearly on an osteoarthritis X-ray or osteoarthritis knee X-ray. Knowing your stage helps in deciding the right treatment strategy.
Stage 1: Minor Osteoarthritis
- What’s seen on X-ray:
Small bone spur growths (tiny bony projections) may be visible, but the joint space usually looks normal. Cartilage is largely intact. - How it feels:
Very mild or no pain. Often goes unnoticed. - Solutions:
- Maintain a healthy weight to avoid extra pressure on joints.
- Start low-impact exercises like swimming, yoga, or walking.
- Add joint-friendly foods and an osteoporosis diet rich in omega-3s and antioxidants.
- Use over-the-counter pain relievers only if occasional discomfort appears.
- Physical Exercise for Osteoarthritis, Muscle Strengthening Exercises and Early Osteoporosis Physiotherapy Management.
Stage 2: Mild Osteoarthritis
- What's seen on X-ray:
Noticeable bone spurs with slight narrowing of the joint space. Early signs of cartilage wearing down. - How it feels:
More frequent stiffness, especially after sitting for long periods or in the morning. - Solutions:
- Physiotherapy for improving joint strength and flexibility.
- Braces or shoe inserts to reduce stress on the affected joint.
- Lifestyle modifications (avoiding high-impact activities, pacing movements).
- Start preventive medications for osteoarthritis if recommended by the doctor (e.g., NSAIDs in moderation).
- Strength Training and Osteoporosis Knee Exercises.
Stage 3: Moderate Osteoarthritis
- What's seen on X-ray:
Clear joint space narrowing, moderate cartilage loss, and more bone spurs. Bones may start rubbing together in some areas. - How it feels:
Persistent pain during daily activities (climbing stairs, kneeling, walking longer distances). Occasional swelling. Also, there’s a change in the shape of the leg. - Solutions:
- Corticosteroid injections to control flare-ups.
- Viscosupplementation (hyaluronic acid injections) to improve lubrication in the joint and to have stronger pain management for osteoarthritis.
- Stronger Osteoarthritis medications or homoeopathic medicine for osteoarthritis for supportive relief are prescribed.
- Weight loss (if overweight) becomes more critical.
- Activity modification: Avoid high strain, but keep joints moving.
Stage 4: Severe Osteoarthritis
- What’s seen on X-ray:
Drastic loss of cartilage, very little to no joint space left, large bone spurs, and visible bone-on-bone contact. - How it feels:
Severe pain, even at rest. Daily activities become difficult or impossible. Change in the shape of the leg (bowing or knock knees). - Solutions:
- Surgical management of osteoarthritis through Joint replacement surgery (hip or knee replacement is common at this stage).
- Assistive devices, like canes or walkers, can be used to reduce joint stress.
- Post-surgery physiotherapy to regain mobility.
- Strong pain management support.
This stage is where an osteoarthritis specialist may recommend advanced care, especially in major cities like consulting a rheumatologist in bangalore.
The above structured approach gives clarity on what the best treatment is for osteoarthritis at each stage.
How Osteoarthritis Feels (Symptoms & Early Signs)
Symptoms usually begin slowly and get worse with time. Some of the most commonly reported osteoarthritis symptoms include:
Common osteoarthritis symptoms
- Joint pain during or after activity
- Morning stiffness (usually under 30 minutes)
- Reduced flexibility
- Crackling or grinding sounds
- Mild swelling around joints
Recognising the above symptoms can help slow progression with timely osteoarthritis treatment options.
H3 - Joint symptoms that signal an emergency
Seek medical help if you experience:
- Sudden severe swelling and redness
- Joints “locking” or “giving way”
- Inability to bear weight
The above symptoms may also indicate complications and require urgent tests for osteoarthritis or imaging. These may require urgent arthritis treatment in Bangalore from an orthopaedic specialist.
Commonly Affected Joints
- Knees: Pain while walking, climbing stairs, or rising from a chair
- Hips: Pain radiating to the groin or thigh, difficulty bending
- Hands & Fingers: Bony enlargements, weak grip strength
- Spine (neck & lower back): Stiffness, nerve irritation causing tingling in arms/legs
These could mean a flare-up or another urgent joint issue. The above could be early signs of osteoarthritis, and taking early action can significantly slow the disease.
Osteoarthritis Diagnosis: When to Seek Help
To get a proper osteoarthritis diagnosis, your doctor will typically:
- History & Symptoms: When pain started, triggers, and relief methods
- Physical Exam: Checking swelling, tenderness, joint function, and may also include a blood test for osteoarthritis to rule out other conditions
- Osteoarthritis X-rays: Show cartilage loss, narrowed joint space, and bone spurs
- MRI (if needed): Detects early cartilage and soft tissue changes
Don’t ignore symptoms; if stiffness lasts more than a few weeks or pain continues to worsen, consult your doctor. Early detection helps in better management of osteoarthritis.
Effective Osteoarthritis Treatment Options
When we discuss osteoarthritis treatment, we're referring to a multi-layered approach that combines medical, physical, and lifestyle changes.
Lifestyle, Exercise & Physical Therapy
Regular low-impact activities like walking, swimming, or tai chi and a little more self-care or any kind of physical exercise during osteoarthritis can help strengthen the muscles around joints. A strong support system for your joints reduces pain and stiffness.
You may also benefit from:
- Resistance band training
- Balance and posture exercises
- Custom orthotics or shoe inserts
- PRP & Viscosupplementation Injection
Start slowly, and always under the guidance of physical therapy for arthritis professionals.
Supplements, Diet & Alternative Therapies
Your diet plays a key role in joint health. The ideal osteoarthritis diet is rich in:
- Dietary supplement for Osteoarthritis, like Omega-3 fatty acids (from flaxseeds, fish, walnuts)
- A customised diet for osteoarthritis, which includes antioxidants (berries, green leafy vegetables)
- Whole grains and low-fat dairy
Some also try turmeric, collagen, or glucosamine for slowing cartilage degeneration, though evidence varies. Acupuncture, massage therapy and alternative treatment for osteoarthritis can provide temporary relief.
Medical & Surgical Solutions
Over-the-counter osteoarthritis medications (glucosamine, collagen supplements, chondroitin sulphate), corticosteroid injections, and hyaluronic acid shots are commonly prescribed. For severe cases, surgery might be the best option. Besides that, new osteoarthritis medications are being studied for cartilage protection.
Osteoarthritis surgery may include:
- Total joint replacement (hip/knee) or osteoporosis knee treatment, depending on severity
- Partial joint resurfacing
- Arthroscopy for cleaning damaged cartilage
These options fall under broader arthritis treatment options in Bangalore available today.
Smart Modifications to Make Daily Life Easier
Small lifestyle upgrades can reduce strain on joints. Try:
- Grab bars in bathrooms
- Non-slip mats
- Electric jar openers
- Elevated toilet seats
- Ergonomic office chairs
These tweaks can dramatically improve your daily comfort and independence.
The Emotional Impact of Living with Osteoarthritis
Living with osteoarthritis isn’t just about aching joints or limited mobility; it reshapes how people experience daily life. Pain that lingers day after day can gradually erode not only physical energy but also emotional resilience.
1. The frustration of limitations
Imagine wanting to play with your child, climb stairs without stopping, or go for a walk with friends, but realising your body doesn’t cooperate. This constant reminder of “can’t do” often leads to frustration, self-doubt, and even guilt.
2. The hidden weight of chronic pain
Unlike a visible injury, osteoarthritis pain is invisible. Many patients describe how difficult it is for others, family, colleagues, or even doctors at times, to see or fully understand the depth of their suffering. This invisibility often leads to feelings of being dismissed or misunderstood.
3. Loneliness and social withdrawal
Chronic pain often forces people to cancel plans or avoid outings that involve standing, walking, or travelling. Over time, this can lead to isolation. Some people fear being a burden, while others quietly pull back from social circles, worsening the cycle of loneliness.
4. The link between pain and mental health
Research shows that people with osteoarthritis are more prone to depression and anxiety. Pain signals from the body constantly engage the nervous system, keeping stress levels high. The result is a mental toll that can feel just as overwhelming as the physical one.
5. Coping strategies that make a difference
It’s important to acknowledge that emotional struggles are not a sign of weakness; they are part of the disease. Seeking help from mental health professionals, joining support groups, practising mindfulness, or even talking openly with loved ones can lighten the load. More and more, doctors now encourage a holistic approach: treating both the body and the mind.
Questions to Ask Your Orthopaedic Doctor
Before your next appointment, go in prepared:
- What stage is my osteoarthritis?
- What lifestyle changes will help most?
- Are injections or osteoarthritis medications right for me?
- Should I consider surgery yet?
- What are the risks of doing nothing?
A clear action plan helps you feel more in control of your joint health.
Habits to Maintain for Strong Joint Health
Prevention is possible. Wondering how to prevent osteoarthritis? Build lifelong habits like:
- Maintaining a healthy weight
(Explore weight loss for arthritis if needed) - Staying physically active
- Practising joint-friendly yoga
- Drinking plenty of water
- Avoiding high heels or poorly cushioned footwear
Daily consistency beats short-term fixes.
Conclusion
Osteoarthritis cure might not exist, or it may be a lifelong condition, but it doesn’t have to define your life. With the right tools, education, exercise, nutrition, and expert care, you can keep doing what you love, pain-free.
Ready to take control of your joint health? Start small. Be consistent. And always stay curious. And in case you’re struggling, consult a trusted specialist. Cities now have expert clinics; finding the right doctor or osteoarthritis specialist could change your life.
FAQs
1. Can anything reverse osteoarthritis?
Sadly, no. While there’s no permanent cure for osteoarthritis, early intervention and consistent treatment can slow down the progression of osteoarthritis and improve quality of life.
2. How can I tell if my joint pain is osteoarthritis?
The best way is to consult a doctor for a test for osteoarthritis. Typical stages range from mild osteoarthritis with little pain to severe bone-on-bone friction.
- Minor – no pain
- Mild – minor stiffness
- Moderate – significant cartilage loss
- Severe – bone-on-bone friction and chronic pain
3. Is walking good for osteoarthritis?
Yes, walking along with strengthening exercises will help. It improves flexibility and strengthens the muscles around joints. Only walking will hamper it; more. Just wear proper shoes and avoid rough surfaces.
4. Will I ever need surgery?
Not always. Osteoarthritis Surgery is only recommended when pain is constant and mobility is severely reduced.
5. How can I reduce flare-ups?
Stick to an osteoarthritis diet, take approved osteoarthritis dietary supplement options, and follow your care plan. Maintain a healthy weight, practice low-impact exercises (like swimming or cycling), use hot/cold therapy, and protect your joints during activity. With proper lifestyle measures, you can reduce the complications of osteoarthritis and live more comfortably.


 Neurosciences
Neurosciences Bariatric Surgery
Bariatric Surgery